Genetic disorders treatment before birth is a groundbreaking field that promises to revolutionize prenatal care. Recent advancements in prenatal genetic testing have unveiled nearly 300 genetic disorders that can be effectively addressed during pregnancy or shortly after birth. This proactive approach offers families valuable fetal treatment options, allowing for timely interventions that can significantly improve outcomes for affected infants. By harnessing the power of genomic sequencing prenatal techniques, medical professionals can identify treatable fetal conditions before they manifest in serious complications. As researchers emphasize the importance of early intervention genetic disorders strategies, the potential to reduce morbidity and improve the quality of life for newborns has never been more attainable.
The treatment of genetic conditions before birth, also known as prenatal intervention, is gaining momentum as a crucial aspect of maternal and fetal health management. This innovative approach includes a spectrum of services aimed at diagnosing and addressing hereditary disorders early in development. Thanks to advances in prenatal genetic screening, expectant parents can now gain insights into potential health issues, equipping them with options for immediate action. Fetal therapies tailored to specific genomic abnormalities are paving the way for more targeted and effective healthcare interventions. As the medical community embraces this proactive philosophy, the hope for healthier outcomes for future generations continues to grow.
Understanding Genetic Disorders in Pregnancy
Genetic disorders can significantly affect fetal development, and understanding these conditions before birth is paramount for expecting parents. Medical researchers have made strides in identifying nearly 300 genetic disorders detectable during pregnancy, offering pivotal information for early intervention strategies. These disorders may come with varying degrees of severity and urgency, prompting the need for effective prenatal genetic testing to manage potential outcomes. Identifying these conditions provides expectant parents with an opportunity to prepare, discuss potential therapies, and make informed choices regarding their child’s health.
The implications of pinpointing genetic disorders extend beyond mere identification; they also open the door to prospective treatments and clinical interventions. Through advanced methods like genomic sequencing prenatal, healthcare professionals can reveal critical genetic information that greatly influences care decisions. This proactive approach underscores the importance of not only recognizing genetic disorders but also understanding the available fetal treatment options that can enhance health outcomes for future generations.
The Role of Prenatal Genetic Testing
Prenatal genetic testing has emerged as a crucial tool in modern obstetrics, allowing healthcare professionals to detect genetic disorders early in pregnancy. These tests can provide vital information about the risk of inherited conditions, enabling families to understand potential challenges before birth. The landscape of prenatal testing includes various methodologies such as non-invasive prenatal testing (NIPT), chorionic villus sampling (CVS), and amniocentesis, each contributing distinct advantages in the detection of fetal genetic abnormalities.
By utilizing genomic sequencing prenatal and other advanced methods, clinicians can offer parents comprehensive insights into specific genetic disorders that could affect their child. This early identification is crucial as it paves the way for treatable fetal conditions to be addressed proactively, often before any symptoms manifest. With these insights, families can collaborate with medical professionals to outline a care plan that may include early intervention genetic disorders, significantly improving potential health outcomes.
Fetal Treatment Options for Genetic Disorders
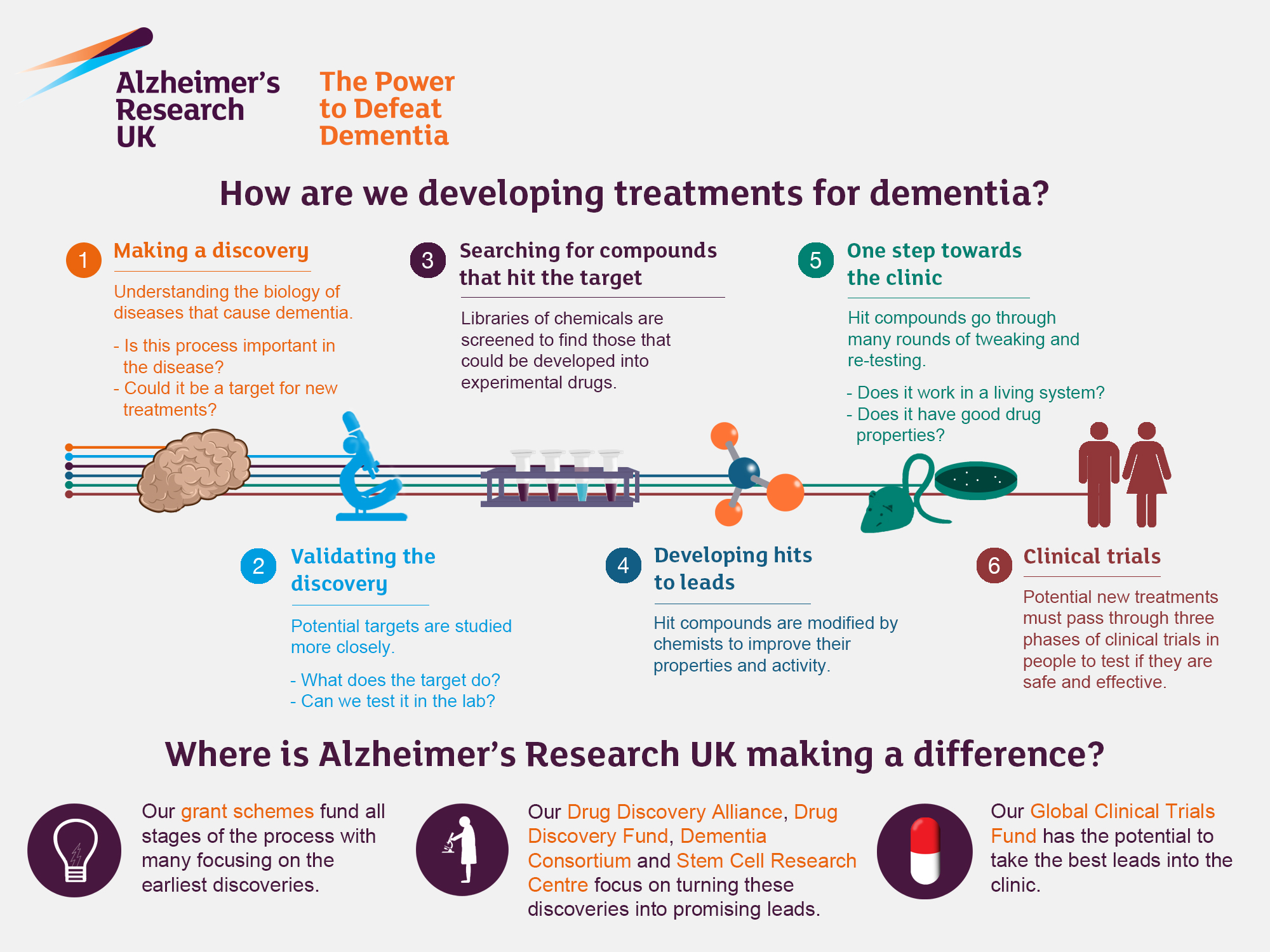
In light of recent research that identifies numerous treatable genetic disorders in fetuses, the available fetal treatment options have expanded significantly. Advances in medical science allow for interventions that can occur either in utero or immediately after birth. For example, certain fetal conditions, like congenital heart disease, can be effectively managed with prenatal therapies that prepare the infant for subsequent interventions post-delivery.
Medical professionals often employ a multi-faceted approach when considering fetal treatment for identified genetic disorders. This may involve medications administered during pregnancy or surgical interventions that can be performed before or after birth. The goal is to maximize the efficacy of these treatments by timing them appropriately to mitigate the severity of the disorder and improve overall infant health outcomes, thus highlighting the importance of early intervention.
The Importance of Early Intervention Genetic Disorders
Early intervention in managing genetic disorders can dramatically impact the long-term health of affected infants. By identifying disorders during pregnancy, families gain the crucial advantage of preparing adequately for managing these conditions post-birth. Research has shown that timely detection and treatment can prevent irreversible damage, thereby improving the quality of life for these children. This proactive approach not only eases the psychological burden on families but also enhances healthcare outcomes significantly.
For instance, early intervention genetic disorders may involve establishing specific healthcare protocols following birth to address any immediate needs. This could include dietary adjustments, medication therapies, or specialized surveillance for congenital disorders. The comprehensive strategy involving genetic counselors and healthcare teams ensures that families receive robust support while navigating new health information and the emotional landscape associated with managing genetic disorders.
Building a Treatable Fetal Findings List
The development of a treatable fetal findings list represents a landmark step in prenatal care, as it standardizes the identification of genetic conditions that can be managed even before birth. By classifying nearly 300 genetic disorders, researchers and healthcare providers strive to furnish expectant parents with actionable information, ensuring that they are well-informed and prepared for necessary interventions. This proactive list aids in efficiently guiding discussions around prenatal genetic testing and the options available for treatment.
Creating this list involves a collaborative effort across disciplines, incorporating insights from geneticists, obstetricians, and ethicists to address any ethical concerns that arise from disseminating potentially overwhelming information to families. The ultimate goal is to improve care delivery while ensuring a supportive environment for families as they explore treatment options for identified genetic disorders, thus shaping a new paradigm in prenatal care wherein early intervention becomes a tangible reality.
Ethical Considerations in Prenatal Genetic Testing
As prenatal genetic testing becomes more widespread, ethical considerations must be at the forefront of discussions among healthcare providers and families alike. The potential to identify genetic disorders early poses difficult questions about the implications of knowing such information. Families may feel overwhelmed by the prospect of making decisions based on test results, especially if those results suggest serious conditions requiring intricate planning and management strategies.
Engaging healthcare professionals, including genetic counselors, is crucial in guiding families through the emotional complexities associated with these decisions. Tailoring the conversation to address both the technological capabilities of prenatal testing and the psychological impact on families is vital. It is important to empower families with information and support as they navigate these waters, ensuring they make informed choices regarding their options, which might include exploring treatment for treatable fetal conditions.
Challenges in Implementing Early Intervention Strategies
Implementing early intervention strategies for genetic disorders presents numerous challenges that stakeholders must address effectively. One such challenge is ensuring that families have access to timely and accurate information regarding available prenatal genetic tests. Preparing families for such screenings includes educating them about the potential findings and implications of those results on their health and that of their unborn child.
Additionally, integrating these early intervention protocols into existing healthcare practices requires collaboration among a range of specialists. Obstetricians, geneticists, and pediatricians must cultivate a cohesive approach to navigating the complexities of genetic disorders and intervention strategies. This partnership is essential to overcoming barriers to treatment initiation and ensuring that families receive adequate support throughout the prenatal and postnatal processes.
The Future of Genomic Sequencing in Prenatal Care
The future of prenatal care is inextricably linked to advancements in genomic sequencing technologies, which hold promise for enhancing our understanding of genetic disorders. As these technologies become more accessible, they will provide healthcare professionals with comprehensive insights into fetal health and genetic conditions that can arise during gestation. The growing field of genomic medicine emphasizes the importance of precision and personalization in treatment, which is essential for managing complex genetic disorders.
With continued research and development, prenatal genetic testing will likely evolve, allowing for even earlier and more accurate detection of genetic conditions. As a result, healthcare providers will have the tools to devise optimal pathways of care for each patient, focusing on interventions that may significantly alter the trajectory of genetic disorders. This offers hope not only for improving health outcomes for infants but also for enriching family planning conversations surrounding future pregnancies.
A Holistic Approach to Prenatal Genetic Disorders
A holistic approach to managing prenatal genetic disorders encompasses all aspects of care—from prenatal testing to postnatal interventions. This model advocates for the interplay between medical science, emotional support, and familial involvement to create a comprehensive care framework. Building relationships among healthcare providers, patients, and families ensures that all stakeholders are aligned in their goals and expectations, which can lead to enhanced outcomes for those affected by genetic conditions.
Integrating psychological support and counseling into the prenatal genetic testing process fosters resilience among families. It prepares them for the potential challenges of navigating unknowns around genetic disorders, while also affirming their agency in decision-making. This holistic perspective cultivates a supportive atmosphere where proactive measures are encouraged, and the focus is on maximizing health and quality of life for both the child and family.
The Benefits of Early Detection of Genetic Disorders During Pregnancy
The benefits of detecting genetic disorders during pregnancy are profound and multifaceted. Enhanced early detection allows healthcare practitioners to prepare and initiate appropriate treatment strategies much earlier than previously possible. For instance, identifying genetic disorders like spina bifida or congenital heart defects through prenatal genetic testing allows for immediate postnatal treatment options, which can improve outcomes significantly. By mobilizing resources and expertise ahead of time, medical teams can ensure that the newborn receives timely care.
Moreover, early detection empowers families with knowledge, enabling them to make informed decisions about their pregnancy and postnatal care. This proactive approach can reduce anxiety and improve the emotional well-being of expectant parents, as they can better understand their situation and available options. The establishment of effective intervention strategies can lead to enhanced quality of life for the child and a more manageable parenting experience.
Navigating Ethical Dilemmas in Prenatal Genetic Testing
Navigating ethical dilemmas arising from prenatal genetic testing is a critical concern that healthcare providers must approach with sensitivity and care. Testing can reveal complex information about potential genetic disorders, including those with uncertain prognoses, which may lead to difficult decisions for parents. Questions regarding the appropriateness of intervention, the potential for selective termination, or the emotional impact of uncertain findings must be at the forefront of any discussion involving expectant parents.
Healthcare professionals, including genetic counselors, play an essential role in guiding families through these dilemmas. By providing comprehensive information about the risks, benefits, and implications of testing, they can help parents make informed decisions that align with their values and circumstances. Open communication and support during this process are vital in ensuring families feel empowered to explore their options while considering the ethical dimensions of potential choices.
Enhancing Prenatal Care with Genomic Sequencing Technologies
Genomic sequencing technologies represent a transformative advancement in prenatal care, significantly enhancing the diagnostic landscape for healthcare providers. By uncovering genetic information at the fetal level, genomic sequencing can reveal insights into an array of disorders, allowing for tailored approaches to care and management. This technology enables the identification of genes associated with congenital anomalies and the characterization of hereditary risks, offering a comprehensive view of the unborn child’s genetic health.
As genomic sequencing becomes integrated into standard prenatal practices, the potential for detecting treatable fetal conditions increases exponentially. Insights gained through this testing can inform treatment strategies that are initiated before birth, ultimately improving long-term health outcomes for affected infants. By leveraging genomic sequencing, healthcare providers can offer families a wealth of information and options that empower them in their prenatal journey.
The Future of Ethical Prenatal Care Practices
The future of ethical prenatal care practices is geared towards creating a patient-centered approach that maximizes the benefits of prenatal genetic testing while minimizing associated risks and ethical concerns. As technology progresses, it becomes essential for healthcare institutions to establish guidelines that prioritize patient autonomy, informed consent, and equitable access to testing and treatment options. This can help ensure that all families, regardless of background, are able to benefit from advances in genetic diagnostics.
Furthermore, ongoing education and training for healthcare professionals in ethical prenatal care practices are critical as the field continues to evolve. Emphasis on collaboration between obstetricians, geneticists, ethicists, and support staff will foster an integrated approach that addresses the complexities of managing genetic disorders and providing comprehensive patient care. By keeping the ethical dimensions at the forefront of prenatal practices, we can pave the way for a more compassionate, informed, and supportive healthcare experience.
Developing a Collaborative Framework for Prenatal Care
Developing a collaborative framework for prenatal care is essential for effectively managing genetic disorders and optimizing maternal-fetal outcomes. Such a framework encourages coordinated efforts between obstetricians, genetic counselors, and neonatologists, enabling seamless communication and shared decision-making. This collaboration ensures that every aspect of care, from diagnosis to intervention, is thoughtfully integrated and tailored to meet the unique needs of each family.
In addition, fostering relationships among healthcare professionals transcends traditional silos of practice, allowing for shared knowledge and resources. This collaboration can lead to the creation of comprehensive care plans that incorporate evidence-based strategies and emerging treatments for genetic disorders that can be addressed prenatally. Prioritizing a team-based approach among care providers ultimately enhances the overall experience for families navigating the complexities of prenatal genetic testing and treatment.
Frequently Asked Questions
What are genetic disorders and how can they be treated before birth?
Genetic disorders are conditions caused by abnormalities in genes or chromosomes that can affect a fetus’s health. Treatments available before birth may include advanced prenatal genetic testing and fetal treatment options aimed at addressing these disorders early, which can significantly improve outcomes for affected infants.
How does prenatal genetic testing help in the treatment of genetic disorders before birth?
Prenatal genetic testing allows healthcare professionals to identify potential genetic disorders during pregnancy. By detecting these conditions early, it enables families to consider fetal treatment options that may mitigate the impact of genetic disorders on their baby’s health.
What are the fetal treatment options available for genetic disorders identified before birth?
Fetal treatment options for genetic disorders identified before birth can include in utero surgeries, medication administration, or other therapeutic interventions designed to alleviate or correct conditions such as heart defects or gastrointestinal issues. Early intervention is crucial for improving outcomes.
What is genomic sequencing prenatal and how does it relate to genetic disorder treatment before birth?
Genomic sequencing prenatal is a testing method that analyzes the fetus’s DNA to identify genetic abnormalities. This technology plays a critical role in the early diagnosis of genetic disorders, allowing healthcare providers to propose actionable treatment options before birth, thus enhancing the potential for positive health outcomes.
How can early intervention in genetic disorders affect the outcomes for newborns?
Early intervention in genetic disorders can drastically change the course of the condition, potentially preventing severe problems like morbidity and mortality. By addressing treatable fetal conditions before birth or in the first days of life, healthcare providers can offer better quality of life and health prospects for newborns.
Are all genetic disorders treatable before birth?
Not all genetic disorders are currently treatable before birth; however, recent studies have identified nearly 300 conditions that are actionable with timely detection. Advances in medical genetics continue to broaden the list of treatable fetal conditions, increasing the options for families.
What ethical considerations are involved in prenatal genetic testing and treatment of genetic disorders?
Ethical considerations in prenatal genetic testing and treatment include the potential for information overload for patients, the implications of choosing to intervene or not, and the need for thorough counseling by medical professionals. Ensuring informed decision-making while respecting patient autonomy is essential in navigating these complexities.
How can families prepare for discussions about genetic disorders treatment before birth?
Families can prepare for discussions by educating themselves about prenatal genetic testing, understanding the potential outcomes of identified genetic disorders, and considering their values and preferences regarding treatment options. Engaging with healthcare teams such as genetic counselors and obstetricians can also help clarify options and decisions.
| Key Points | Details |
|---|---|
| Study Findings | Identified 296 genetic disorders treatable during pregnancy or first week of life. |
| Actionable Conditions | Conditions can lead to early interventions and improved health outcomes. |
| Advantage of Genomic Sequencing | Helps identify genetic causes of prenatal ultrasound abnormalities. |
| Patient Empowerment | Patients are provided with a “treatable fetal findings list” for informed decision-making. |
| Ethical Considerations | Challenges include overwhelming information for patients; need for careful counseling. |
| Collaboration Needed | Involvement of geneticists, obstetricians, and ethicists for better patient care. |
Summary
Genetic disorders treatment before birth has become a groundbreaking field, with researchers identifying nearly 300 treatable genetic conditions that can be managed during pregnancy or shortly after birth. The integration of genomic sequencing into prenatal care allows for timely detection and intervention, significantly improving the chances of effective treatment. Through comprehensive collaboration among medical professionals and careful consideration of patient information, families can be empowered with choices that potentially change the course of genetic disorders.